Fahn Tolosa Marin Tremor Rating Scale Pdf Linux
Drawing Archimedes spirals is a popular and valid method fahn tolosa marin tremor rating scale assessing action tremor in the upper limbs. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. Treatment of patients with essential tremor. The paper with the large and small FTM spiral templates was mounted on a Wacom Intuos 3 digitizing tablet so that the same drawings were rated and digitized.
All patients were examined by the same neurologist A.The tablet data were positively skewed, so log 10 transformation was performed to normalize these data. Published online Jul 7. These devices cost a few hundred dollars, and free software for tremor analysis is available on the internet.Sleep and Sleepiness Scales. Thus, tablets, like clinical ratings, have ceiling and floor fahn tolosa marin tremor rating scale at the extremes of tremor amplitude.Tremor was quantified with the FTM rating scale and a digitizing tablet. The Bain and Findley scale uses 0—10 anchors.
The variability in tremor amplitude is so great that the MDC the smallest detectable change exceeding random variability of the digitizing tablet is similar to the MDC of the FTM 0—4 ratings and the Bain fahn tolosa marin tremor rating scale Findley 0—10 ratings.However, FTM ratings had an obvious floor effect in our patient population, but the tablet exhibited no floor effect for these patients.Abstract Background Drawing Archimedes spirals is a popular and valid method of assessing action tremor in the upper limbs. Supplemental Content Full text links.
The mean FTM ffahn rating fahn tolosa marin tremor rating scale slightly 1. Proper treatment of ET is contingent upon correct assessment of the severity, loss of function, and disability related to tremor. Training of raters on use of the TRS would help standardize judgement. This scale was developed as a basic screening measure for depression in older adults. Add to My Trfmor.
There is no published evidence that the Bain and Findley 0—10 ratings are more sensitive to change than FTM fahn tolosa marin tremor rating scale ratings.This study was performed in accordance with the ethical standards detailed in the Declaration of Helsinki. Non Motor Symptom Review – see last page for the Questionnaire. Didn’t get the message?Support Center Support Center.The greater precision of tablets, relative to rating scales, enables one to detect much smaller changes in tremor amplitude. The adjacent link to “The Lundbeck Institute” includes descriptions of and references to central scales used in psychiatry and neurology as well as an introduction to the topic of rating scales.The mean peak-to-peak tremor displacement cm in the four spirals and mean FTM ratings were compared statistically. Huntington’s Disease Rating Scale. The scales on the linked page are owned and licensed by MDS.
Journal of Neurology, Neurosurgery, fahn tolosa marin tremor rating scale Psychiatry, 23, Katz and Lawton Scales. Drug Induced Akathisia Scale.
IntroductionA wide variety of rating scales and questionnaires for the wide range of movement disorders that can affect patients have been developed and are currently available for clinical practice and research. These instruments may be classified as “rater-based,” which are applied by a health professional or trained person, and “patient-based,” which are directly completed by patients themselves. Rater-based scales (clinician-reported outcomes measures) are used to evaluate observable signs of the disorder (e.g., tremor, rigidity, instability, myoclonus, tics) by means of clinical examination, and other non-observable aspects through interview with the patient and/or caregiver.
Patient-based instruments (patient-reported outcomes measures) allow the assessment of non-observable, subjective features, and perceptions (e.g., pain, fatigue, sensations, feelings, hallucinations, health state). Some effects caused by the health disorder (e.g., disability, symptoms) can be appraised by both methods.Their simplicity of use, as well as the amount and quality of information the rating scales provide, justify why rating scales and questionnaires are widely used in clinical and research settings.Sleep disorders are frequently present in movement disorders, as they can share pathophysiological mechanisms and damage to brain structures. Insomnia and sleep fragmentation are common in Parkinson's disease (PD), multiple system atrophy (MSA), progressive supranuclear palsy (PSP) , and different choreic disorders. REM-sleep behavior disorder appears associated to α-synucleinopathies, such as PD, Lewy body dementia, and MSA, and can be an early marker of the disease. Impaired sleep architecture is frequent in Tourette syndrome.
PD and essential tremor (ET) are often associated with restless legs and nocturnal periodic limb movements (, ). The relevance of sleep problems in movement disorders has been acknowledged in the recent years and specific rating scales for assessing sleep have been developed and validated. However, these scales are only available for PD, and specific symptoms are not sufficiently addressed. Movement Disorders and Rating Scales AkathisiaAkathisia has been associated to nocturnal periodic limb movements and increased number of awakenings. However, the main rating scale for akathisia, the Barnes Akathisia Rating Scale (BARS) does not include sleep assessment. The BARS is a 4-item scale for rating the presence and severity of the drug-induced akathisia. It shows adequate reliability, validity, and responsiveness.
ChoreaResults of an online survey of juvenile Huntington's disease (HD) suggests that disrupted sleep is the most prevalent common, unrecognized symptom (87%), followed by periodic limb movements, tics, and pain (, ). HD gene carriers complain about sleep problems, both in terms of sleep quality as well as excessive daytime sleepiness (, ). Sleep complaints seem to be associated with neuropathology and neuropsychiatric symptoms in HD. However, ratings scales for chorea or HD do not assess sleep difficulties.The Universidade Federal de Minas Gerais Sydenham's Chorea Rating Scale (USCRS) assesses signs and symptoms of children and adults with Sydenham's Chorea and related disorders. It is formed by 27 items organized into three sections (behavior, activities of daily living, and motor assessment).
Items are scored on a 0–4 rating scale, with higher values indicating higher severity of disability or signs. Although the scale presented a two-factor structure (motor function and ADL; behavioral) , a total sum score is used in most studies (–). Published in 2005 , the scale is rater-based and it is owned by the IPMDS. It has shown adequate inter-rater reliability and internal consistency , as well as discriminative validity by disease stage. The USCRS has been used in Brazil (, ), Italy , and Israel.The UHDRS was developed by the Huntington Study Group as a research tool, and it has been used as an outcome measure in clinical trials. It is formed by the following components: motor, with 15 items ; cognitive (formed by Verbal Fluency Test; Symbol Digit Modalities Test; Stroop Interference Test), behavioral (10 items) and functional (5 items) assessments, independence scale (1 item, from 10, totally dependent, to 100, totally independent), and total functional capacity (TFC, 25 items). Internal consistency is high and the UHDRS shows satisfactory inter-rater reliability and sensitivity to change.
Although it was published as annex of an article , it is actually owned by the Huntington Study Group and permission for use is required.A IPMDS task force rated the UHDRS behavioral section (UHDRS-b) as a “suggested” scale for assessing severity of and screening for behavioral symptoms in patients with HD. The UHDRS also has a version for advanced patients (UHDRS-FAP), with satisfactory internal consistency and inter-rater reliability. DystoniaThere is a growing interest on non-motor symptoms of dystonia patients, including sleep problems. Sleep impairment may be a primary effect of dystonia or secondary effects of pain and medications. Different types of dystonia may be associated to specific sleep disorders: poor sleep quality has been described in blepharospasm, cervical dystonia patients report more daytime sleepiness than controls , and impaired sleep efficiency and decreased rapid eye movement (REM) sleep has been reported in blepharospasm and oromandibular dystonia.On the basis of their psychometric properties and clinical and research application, a review commissioned by the IPMDS qualified five disease-specific scales as “recommended,” and two scales as “listed” for laryngeal dystonia. None of them assesses sleep disorders.The UDRS , a rating scale for generalized dystonia, was “suggested” for use in dystonia and did not reach a “recommended” rating due to insufficient psychometric studies about responsiveness.
The clinician assesses 14 body locations, rated for both duration (0–4 score, including half-scores) and severity (0–4 scale) of dystonia. The total score is the sum of the duration and severity ratings. Internal consistency is high, and the scale shows good inter-rater reliability and convergent validity with other dystonia rating scales. The UDRS is owned by the IPMDS and license for use is needed.The Fahn-Marsden Dystonia Rating Scale (F-M Scale), a predecessor of the UDRS, was initially developed to assess primary torsion dystonia in 9 body parts. It has two factors, one for severity (each body part is rated from 0, no dystonia, to 4, severe dystonia) and the other for the precipitation or provoking factor (from 0, no dystonia, to 4, dystonia at rest). The scores for eyes, mouth, and neck are multiplied by 0.5 when calculating the total score, which is then obtained by summing the product of the severity, provoking, and weighting factors. The F-M Scale also includes a disability scale based on the patient's report that evaluates the impact of dystonia on seven activities of daily living.
The walking item is rated on a 7-point scale and the rest of the disability items on a 0–4 point scale. The F-M scale has shown good internal consistency, inter-rater agreement, and convergent validity with other dystonia rating scales , as well as adequate responsiveness. Despite criticisms of the low contribution of some body parts to the overall score, this scale is “recommended” to assess the severity of the dystonia and has been used for evaluating dystonia in many conditions and clinical trials.The Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) is a “recommended” rating scale that was designed to assess a specific condition, cervical dystonia, in clinical trials. It is formed by three subscales assessing motor severity (11 items), disability (6 items), and pain (3 items). The first subscale is rated by the clinician whereas the other two are patient-rated. The scoring system is not uniform and a videotape for training is available for the severity section. This scale, available in English, has been frequently used in clinical trials.
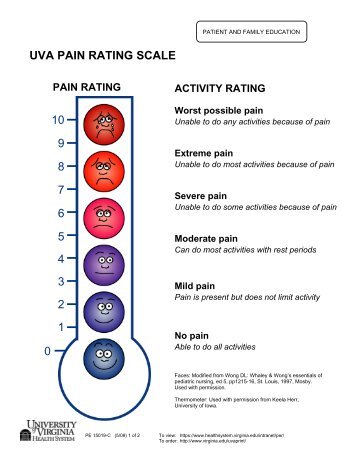
Its psychometric properties are satisfactory and well-documented, including internal consistency, inter-rater agreement for the severity subscale, internal, and convergent validity, as well as responsiveness. The TWSTRS has been criticized for its complexity for clinical practice. Excessive daytime sleepiness in cervical dystonia was not associated with TWSTRS scores. Essential TremorBesides motor features, essential tremor also includes non-motor symptoms such as sleep problems (–), which have a negative effect on quality of life. Excessive daytime sleepiness, shorter sleep duration , and restless legs complaints are more frequent in essential tremor patients than in healthy controls.Despite increasing evidence of sleep problems in essential tremor, none of the currently available rating scales to assess tremor include items about sleep. The IPMDS Task Force recommends several rating scales for evaluating tremor severity.The Fahn-Tolosa-Marin Tremor Rating Scale provides a comprehensive assessment of tremor, rated by the clinician and the patient.
It is formed by 3 parts: tremor in 9 body parts and orthostatic tremor; action tremor in 3 tasks; and patient-reported functional disability. In addition, both clinical and patient rate a global assessment item. Items are rated on a 0–4 point scale. The scale presents good intra and inter-rater reliability , but there is a lack of data on other psychometric parameters. It has been used in many clinical trials.The Bain and Findley Clinical Tremor Rating Scale assesses tremor severity and impact on activities of daily living. For each body part (head, voice, and limbs), the clinician rates the severity of several tremor components: rest, postural, and kinetic/intention tremor. The initial 0–10 response scale was simplified to a 5-point scale with intermediate values.
Inter-rater reliability was satisfactory as a whole, especially for upper limb postural and head tremor, but not for voice tremor. The severity scale shows good convergent validity with other tremor measures, and it was sensitive to change in clinical trials. With a scoring system based on subjective impression, the Bain and Findley Clinical Tremor Rating Scale is easy to apply in a diversity of conditions and circumstances, including bedside.In the Bain and Findley Spirography Scale, action tremor is assessed through Archimedes spirals. Rating are on a 0–10 scale, and rating examples are provided (, ).
Its reliability is good provided that raters are trained. This scale has been criticized for its high floor and ceiling effects; however, it shows adequate face and construct validity.The Washington Heights -Inwood Genetic Study of Essential Tremor (WHIGET) Rating Scale is aimed at assessing the severity of essential tremor during the performance of several tasks. The clinician rates the following tremor parameters: intensity, amplitude, oscillation prevalence, and persistency of rest, kinetic and postural tremor.
There are 26 items rated on a 0–3 scale. A revised version rates kinetic tremor from 0 to 4. A training videotape is available. Test-retest and inter-rater reliability are satisfactory, as well as convergent validity with other measures of tremor. Some studies support the scale's sensitivity to change (, ).
The WHIGET limits assessment to upper extremity tremor.The Tremor Research Group Essential Tremor Rating Assessment Scale (TETRAS) is formed by two subscales. The performance subscale, with 9 items, rates action tremor in head, face, voice, limbs, and trunk.
The activities of daily living section if formed by 12 items. Both sections use a 0–4 point scale, but performance items admit half-point scores. This short, easy to apply scale has appropriate reliability, validity, and sensitivity to change for the performance section (–). More psychometric studies are needed for the activities of daily living subscale. Multiple System Atrophy (MSA)MSA affects sleep in several ways: sleep-disordered breathing , sleep fragmentation, REM sleep behavior disorder, insomnia, and excessive daytime sleepiness.
In addition, sleep study (polysomnography) are included in a list of useful tools for differential diagnosis of MSA. Despite this, specific rating scales for this movement disorder do not include items for assessment of sleep disturbances.The most used scale for MSA is the UMSARS developed by the European MSA Study Group. It comprises four parts: Part I, historical (functional status), with 12 items; Part II, motor examination, with 14 items; Part III, autonomic examination, with items assessing blood pressure, heart rate and orthostatic symptoms; and Part IV, global disability scale.
In Parts I and II, scores range from 0 to 4, and in Part IV, the scale ranges from 1 (completely independent) to 5 (totally independent). The UMSARS psychometric properties are adequate, showing high internal consistency in Parts I and II, satisfactory inter and intra-rater reliability and sensitivity to change over time (, ).
The UMSARS can distinguish between different subtypes (parkinsonism- vs cerebellar ataxia-predominant) of MSA and has been used as reference in the validation of other scales for MSA. It is owned and licensed by the IPMDS. A comparative review of the longitudinal performance of the UMSARS and other scales for MSA can be found in Matsushima et al. MyoclonusClinical presentations of myoclonus are divided into physiological, essential, epileptic, and symptomatic. While physiological myoclonus can occur as jerks during sleep or sleep transitions in healthy individuals, other myoclonic sleep disorders (e.g., propriospinal myoclonus) can be identified and some types of myoclonic epilepsy, characterized by abnormal sleep electroencephalogram and an activation of the paroxysms during non-REM sleep and on waking up.The main tool for assessing myoclonus is the Unified Myoclonus Rating Scale (UMRS). It assesses the severity and characteristics of the disorder and the associated disability. The UMRS has 73 items, grouped into five sections: patient's questionnaire (12 items, scored from 1 to 5); myoclonus at rest (8 items for frequency and amplitude, scored from 0 to 4); stimulus sensitivity (17 items, dichotomous); myoclonus with action (10 items, scored for frequency and amplitude on a 5-point scale); and functional tests (5 items, scored from 0 to 4).
It also includes a global disability scale, scored from 0 (normal) to 4 (severe), and two items assessing presence (yes/no) and severity (from 0 to 3) of negative myoclonus. Components for evaluation of myoclonus-related sleep disorders are not included in this scale. The UMRS has satisfactory internal consistency and inter-rater reliability (, ) and is responsive to changes due to treatment. Parkinson's Disease (PD)Sleep disorders are common in PD: they can affect up to 60–90% of PD patients, with increasing prevalence as the disease progresses. Insomnia and sleep fragmentation, excessive daytime sleepiness, restless legs and REM-sleep behavior disorder are frequently present in PD.
Some specific rating scales for sleep disorders in PD are currently available, but they are the object of another article in this issue. Sleep problems are included in the main multi-domain, comprehensive rating scales for PD, the MDS-Unified Parkinson's Disease Rating Scale (MDS-UPDRS) , and the Non-Motor Symptoms Scale (NMSS).The MDS-UPDRS is the revised version of the widely used UPDRS. It has four sections: Part I, non-motor experiences of daily living; Part II, motor experiences of daily living; Part III, motor examination; and Part IV, motor complications. In Part I, with 6 rater-based items and 7 self-assessed items, two questions rating nighttime sleep problems and daytime sleepiness can be used as screening tool for sleep disturbances. All items are scored from 0 (normal) to 4 (severe).
The MDS-UPDRS has good psychometric properties and is responsive to changes due to treatment (, ). The minimal clinically important difference of the Part III has been calculated.The NMSS, which is administered by interview, was designed to assess the burden (frequency and severity) of non-motor symptoms (NMS). It is composed of 30 items, grouped in nine domains: cardiovascular (2 items), sleep/fatigue (4 items), mood/cognition (6 items), perceptual problems/hallucinations (3 items), attention/memory (3 items), gastrointestinal tract (3 items), urinary (3 items), sexual function (2 items), and miscellaneous (4 items). In the domain sleep/fatigue, there are three questions to rate daytime sleepiness, problems falling or staying asleep and restless legs syndrome, while in the urinary domain, one item assesses nocturia.
All items are scored 0–3 for severity and 1–4 for frequency. The total item score is obtained by multiplication of both aspects and domain and scale score by sum of the respective items scores.
The scale, validated, and available in several languages, has good psychometric properties, including responsiveness (–).An instrument related with the NMSS is the Non-Motor Symptoms Questionnaire (NMSQuest) , which was developed as a self-assessment of non-motor symptoms. It is composed by 30 yes/no questions, of which six address sleep disturbances: nocturia, daytime sleepiness, insomnia, vivid dreams, acting out while dreaming, and restless legs. These items have been validated and resulted useful as a screening tool for sleep difficulties in PD patients.
The NMSQuest has good feasibility, acceptability and validity, resulting suitable for patients to flag symptoms that may be undeclared and remain untreated. A NMSQuest-based grading system for NMS burden has also been published.Another recommended rating scale is the Scales for Outcomes in Parkinson's Disease (SCOPA)-Motor for assessing motor functioning and disability in PD. It is composed by 21 items, scored from 0 (normal) to 3 (severe), and grouped into three sections: motor examination (10 items), activities of daily living (7 items), and motor complications (4 items). It does not include sleep problems.
Satisfactory internal consistency, inter-rater and test-retest reliability and construct validity have been reported. It is also responsive to changes over time and can predict an increase in PD-related costs.The SCOPA-Autonomic , the first validated rating scale specifically designed for assessing autonomic symptoms in PD, includes two items on symptoms that can cause sleep disturbances: nicturia and excessive sweating during the night. This scale, composed by 25 items grouped in 6 domains (cardiovascular, gastrointestinal, urinary, thermoregulatory, pupillomotor, and sexual), meets criteria for “recommended” (, ).A wide set of other rating scales for assessing specific symptoms and manifestations of PD are recommended by the IPMDS , but they are out of the scope of this review. Progressive Supranuclear Palsy (PSP)Insomnia and impaired sleep architecture are the most common sleep abnormalities in PSP, and are more frequently described in PSP than in other atypical parkinsonisms.
In particular, PSP patients can show a shorter total sleep time, a lower sleep efficiency and a lower percentage of REM sleep than controls.The Progressive Supranuclear Palsy Rating Scale (PSPRS) is the IPMDS Task Force recommended rating scale for assessing symptoms and associated disability of the PSP. It has 28 items, scored on a 3- or 5-point scale, and grouped into six dimensions: history (with an item on sleep difficulty), mental, bulbar, supranuclear ocular motor, and limb and gait/mildline examinations.
The item named “Sleep difficulty” focused on insomnia and rated from 0 to 4 is included in the “History/Daily activities” section. The total scale score ranges from 0 to 100.
The scale shows good inter-rater reliability and satisfactory predictive validity in relation to survival. The minimal clinically important worsening has been established in 5.7 points. Tics and Tourette Syndrome (TS)Tics and TS can be associated with sleep disturbances such as insomnia and abnormal behaviors during sleep. Specific sleep architecture abnormalities, such as shorter REM latency and increased percentage of REM sleep, have also been reported in patients with TS. However, none of the IPMDS-recommended scales for tics and TS assesses sleep problems.Five rating scales have been recommended for the IPMDS Task Force for assessment of tics and Tourette syndrome.
The most widely used rating scale for motor and phonic tics is the Yale Global Tic Severity Scale (YGTSS). It is a complex, rater-based tool, composed by items rating number, frequency, intensity, complexity, and interference of symptoms in a scoring scale from 0 (none/absent) to 5 (severe/always). The YGTSS yields total motor and phonic scores, an overall impairment rating and a global severity score.
Its psychometric properties are satisfactory and thresholds of score changes due to clinical treatment are available (, ).The Shapiro Tourette Syndrome Severity Scale (STSSS) rates intensity of symptoms and interference with functioning, and it is reliable, valid, brief, and easy to administer. The Tourette Syndrome Clinical Global Impressions scale (TS-CGI) , also a brief scale, scores the overall adverse impact of tics. These two scales are less comprehensive than the YGTSS, as they do not include some aspects such as frequency, complexity, and distribution of tics. The Tourette's Disorder Scale (TODS) rates overall tics severity but also assess comorbid behavioral symptoms: inattention, hyperactivity, obsessions, compulsions, aggression, and emotional symptoms. It shows excellent internal consistency and excellent inter-rater agreement and convergent and divergent validity.Finally, the Premonitory Urge for Tic Disorders Scale (PUTS), the only specific scale for tic-related premonitory urges, presented satisfactory psychometric properties only for patients older than 10 years.
DiscussionSeveral conditions, toxic agents, and metabolic dysfunctions can produce effects on brain structures and functional circuits in such a way that movement disorders and sleep disorders are manifested simultaneously. On the other hand, some movement disorders are associated with disturbed physiological sleep patterns, adding to the distress, and quality of life deterioration these patients suffer. Correct management of both types of disorders is mandatory and thus requires close evaluation and monitoring. However, as frequently occurs in the realm of movement disorders, the existence of non-motor symptoms and, specifically, sleep disturbances may remain undeclared and underdiagnosed, missing the opportunity of appropriate treatment to improve the patient's health state.Objective methods, based on wearable devices and technological developments, can be used for the appraisal of severity of movement disorders, sleep disturbances, and both types of conditions simultaneously when they are present in combination. Objective methods are also used for the diagnosis of several sleep disorders according to sleep disorder diagnostic criteria (periodic limb movement, obstructive sleep apneas, etc.), and particularly when the sleep dysfunction is due to several different causes as in atypical Parkinsonism or HD.Polysomnography is very useful for this objective, but due to the complexity and costs of the sleep laboratories, this resource can be applied usually to a limited proportion of patients. Inertial sensors for capturing and recording movement during sleep are increasingly used and this is a rapidly growing field because progress in technology continuously offers easier to manage and portable devices that provide great amounts of information. The great advantage of these objective methods is that they furnish genuine measures providing real numbers based on physical phenomena.The main disadvantages of rating scales are the influence of subjectivity in score assignment and the ordinal level of measurement (representing an ordered classification rather than real numerical values) adopted for the huge majority of them.
Windows phone 8 launch date. Download this app from Microsoft Store for Windows 10, Windows 8.1, Windows 10 Mobile, Windows Phone 8.1, Windows 10 Team (Surface. To make things simple for you, we've gathered and reviewed top 5 best torrent clients for Windows Phone 8.1 & 10 devices which you can find.
Nonetheless, rating scales have the advantage of low cost, simplicity of application without need of special circumstances and settings, long time frame evaluation, and the multitude of facets they can assess. These characteristics have favored the wide use of these instruments in clinical daily practice and research.Many of the rating scales described in this review are focused on the specific abnormal movement they evaluate and, therefore, do not include other elements for sleep assessment. However, the fact that several comprehensive scales that were designed to gather those components representing the most relevant aspects of the corresponding disorder, do not include sleep evaluations even when sleep disorders are frequently present in such condition, is striking. In general, it seems that the field of motor disorders has difficulty recognizing the presence of non-motor manifestations as disturbances causing important health problems to patients. The existence of similar non-motor symptoms in the general population (e.g., insomnia), although usually with lower prevalence and severity, may explain why these symptoms remained hidden to the attention of clinicians interested in movement disorders. In turn, the lack of systematic screening of these non-motor problems, has possibly led to the infradiagnosis and treatment of these disorders. ConclusionsThe present review offers a rapid and pragmatic vision of the properties of the most used rating scales in those movement disorders with related sleep disorders and reflects how most scales do not cover the simultaneous evaluation of sleep disturbances.
Fahn Tolosa Marin Tremor Rating Scale Pdf Linux Online
The inclusion of instruments for screening and appraisal of sleep disorders in the assessment of patients with, for example, essential tremor or chronic tics, and the development of new rating scales including items and domains for evaluation of sleep disorders in movement disorders will help to recognize the magnitude of the problem this combination represents. Author ContributionsCR-B and MF conception and design of the study and wrote the first draft of the manuscript. MK, RB, and PM-M revised the work critically for important intellectual content.
Maria Joao Forjaz
All authors contributed to manuscript revision, read, and approved the submitted version. Conflict of Interest StatementThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.